Bromance can do you good, according to a research from the University of California, Berkeley, which noted that the health benefits of male bonding are similar to those of romantic relationships, specifically after stressful situations.
Human studies already showed that social interactions increase the level of the hormone oxytocin in the brain, and that oxytocin helps people bond and socialize more, increasing their resilience in the face of stress. This, in turn, leads to longer, healthier lives. These findings were confirmed by studies of male-female rat pairs and other rodents, such as monogamous prairie voles.
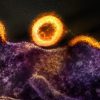
In “Moderate Stress-Induced Social Bonding and Oxytocin Signaling are Disrupted by Predator Odor in Male Rats“, Sandra E. Muroy, Kimberly L.P. Long, Daniela Kaufer and Elizabeth D. Kirby looked at same-sex conspecifics — particularly males — stress effects on social bonding as these are “less understood and often associated with aggression and social unrest”. they specifically “sought to investigate if a moderate stressor — 3 h of acute immobilization — impacts social-support behaviors differently when experienced in a neutral versus more innately threatening context (i.e. paired with predator odor).”
They found that moderate stress increased social support-seeking behavior in rat cagemates and facilitated long-term sharing of a limited water resource, decreased aggression, and strongly defined dominance ranks (an indicator of home cage stability).
In contrast, experiencing the same stressor in the presence of predator odor eliminated the positive behavioral effects of moderate stress.
“Importantly, hypothalamic oxytocin (OT) signaling increased coincident with stress in a neutral, but not a predator odor, context. Our results define a novel rodent model of divergent stress effects on social affiliation and OT signaling dependent on odor context with particularly strong relevance to stress-related disorders such as PTSD which are characterized by a disrupted ability to seek and maintain social bonds.”
“In times of stress, social support can serve as a potent buffering mechanism that enhances resilience. In humans, stress can promote protective affiliative interactions and prosocial behavior. Yet, stress also precipitates psychopathologies characterized by social withdrawal such as posttraumatic stress disorder (PTSD) and depression,” the authors stated.
“A bromance can be a good thing,” said lead author Kirby. “Males are getting a bad rap when you look at animal models of social interactions, because they are assumed to be instinctively aggressive. But even rats can have a good cuddle – essentially a male-male bromance – to help recover from a bad day.”
Kirby added that having friends is not “un-masculine.”
“These rats are using their rat friendships to recover from what would otherwise be a negative experience. If rats can do it, men can do it too,” Kirby ended.
The study will be published in the journal Neuropsychopharmacology.