A new report by UNAIDS, Power to the people, released in time for the observance of World AIDS Day 2019, shows that where people and communities living with and affected by HIV are engaged in decision-making and HIV service delivery, new infections decline and more people living with HIV gain access to treatment. When people have the power to choose, to know, to thrive, to demand and to work together, lives are saved, injustices are prevented and dignity is restored.
“When people and communities have power and agency, change happens,” said Winnie Byanyima, Executive Director of UNAIDS. “The solidarity of women, young people, gay men and other men who have sex with men, sex workers, people who use drugs and transgender people has transformed the AIDS epidemic—empowering them will end the epidemic.”
The report was launched in Kenya on 26 November by the Executive Director of UNAIDS, the Cabinet Secretary of Health of Kenya and community representatives. It shows that significant progress has been made, particularly in expanding access to treatment. As of mid-2019, an estimated 24.5 million of the 37.9 million people living with HIV were accessing treatment. As treatment roll-out continues, fewer people are dying of AIDS-related illnesses.
“The partnership between government and civil society, together with the meaningful involvement of communities, has allowed us to significantly reduce new HIV infections and AIDS-related deaths,” said Sicily Kariuki, Cabinet Secretary for Health in Kenya. “Communities are the very centre of the AIDS response and are critical to ending AIDS.”
Progress in reducing HIV infections, however, is mixed and 1.7 million people were newly infected with the virus in 2018. New HIV infections declined by 28% from 2010 to 2018 in eastern and southern Africa, the region most affected by HIV. In a promising sign, the incidence rate of HIV among adolescent girls and young women aged between 15 and 24 years in the region declined from 0.8% in 2010 to 0.5% in 2018, a 42% decline. However, young women and girls still bear the brunt of new HIV infections—four out of five new HIV infections among adolescents in sub-Saharan Africa are among girls.
Outside of eastern and southern Africa, new HIV infections have declined by only 4% since 2010. Of increasing concern is the rise of new HIV infections in some regions. The annual number of new HIV infections rose by 29% in eastern Europe and central Asia, by 10% in the Middle East and North Africa and by 7% in Latin America.
“In many parts of the world, significant progress has been made in reducing new HIV infections, reducing AIDS-related deaths and reducing discrimination, especially in eastern and southern Africa, but gender inequality and denial of human rights are leaving many people behind,” said Ms Byanyima. “Social injustices, inequality, denial of citizenship rights and stigma and discrimination are holding back progress against HIV and the Sustainable Development Goals.”
Power together
The report shows that when people and communities have power and agency, change happens. Communities have put rights-based, people-centred principles at the heart of HIV programmes, ensuring that AIDS responses tackle the inequalities and injustices that fuel the epidemic.
Women and girls are the backbone of care support in their families and communities, providing unpaid and often undervalued work in caring for children, the sick, the elderly and the disabled and underpinning fragile social support systems. This must change. The involvement and leadership of communities of women is vital in the response to HIV.
“As a community leader, I am able to relate to people and understand their background better than someone from the outside. I have been living openly with HIV for 25 years, so people come to me with their issues, such as HIV-related stigma, disclosure and adherence. I have never stepped back from this role as I am part of this community,” said Josephine Wanjiru, an HIV community activist in Kiandutu, Thika, Kenya.
The power to choose
Women and girls are demanding integrated contraception and HIV and sexually transmitted infection testing, prevention and care options. Almost 40% of adult women and 60% of adolescent girls (aged 15–19 years) in sub-Saharan Africa have unmet needs for modern contraception.
In several countries in sub-Saharan Africa, young women’s uptake of medicine to prevent HIV—pre-exposure prophylaxis (PrEP)—has been shown to be high in projects that integrate PrEP into youth-friendly health services and family planning clinics and when provision of PrEP is separated from treatment services.
Eleven million voluntary medical male circumcisions to prevent HIV have been performed since 2016, 4 million in 2018 alone in the 15 priority countries.
The power to know
The power to know allows people to keep themselves free from HIV or, if living with the virus, keep healthy. However, people are finding out their HIV status too late, sometimes years after they became infected, leading to a delay in starting treatment and facilitating HIV transmission. In Mozambique, for example, the average time for diagnosis after infection for men was four years.
Adherence to effective treatment suppresses the virus to undetectable levels, keeping people healthy and preventing transmission of the virus. Knowing this allows people living with HIV the opportunity to lead normal lives, confident that they are protecting their loved ones, and confronting stigma and discrimination.
HIV self-testing is now helping more people to find out their HIV status in privacy, breaking the barriers of stigma and discrimination and facilitating linkage to treatment.
Knowledge of HIV among young people is alarmingly low in many regions. In countries with recently available survey data, just 23% of young women (aged 15–24 years) and 29% of young men (aged 15–24 years) have comprehensive and correct knowledge of HIV. Studies show that comprehensive sexuality education does not lead to increased sexual activity, sexual risk-taking or higher infection rates for HIV or other sexually transmitted infections.
The power to thrive
The power to thrive is ensuring that people have the right to health, education, work and a standard of living adequate for health and well-being.
New HIV infections among children have declined by 41% since 2010 and nearly 82% of pregnant women living with HIV are on antiretroviral therapy. However, thousands of children are falling between the cracks. Half of all children born with HIV who are not diagnosed early will die before their second birthday, but, globally, only 59% of HIV-exposed children were tested before two months of age.
In 2018, 160 000 children (aged 0–14 years) became newly infected with HIV, and 100 000 children died from an AIDS-related illness. They died either because they weren’t diagnosed, or because of a lack of treatment—a shocking indictment of how children are being left behind.
Gender inequalities, patriarchal norms and practices, violence, discrimination, other rights violations and limited access to sexual and reproductive health services exacerbate the risk of HIV infection among adolescent girls and young women, particularly in sub-Saharan Africa. Each week, an estimated 6000 young women (aged 15–24 years) are infected with HIV.
In Eswatini, a recent study showed that adolescent girls and young women who experienced gender-based violence were 1.6 times more likely to acquire HIV than those who did not. The same study also showed that the economic empowerment of women and girls helped in reducing new HIV infections among women by more than 25% and increased the probability of young women and girls going back to school and finishing their education.
Key populations are being left behind
Key populations and their partners account for at least 75% of new HIV infections outside of sub-Saharan Africa and are less likely to be on treatment than others. More than one third of key populations do not know their HIV status. Community-led support among gay men and other men who have sex with men is effective in increasing the uptake of PrEP, promoting safer sex, increasing HIV testing rates and supporting treatment adherence.
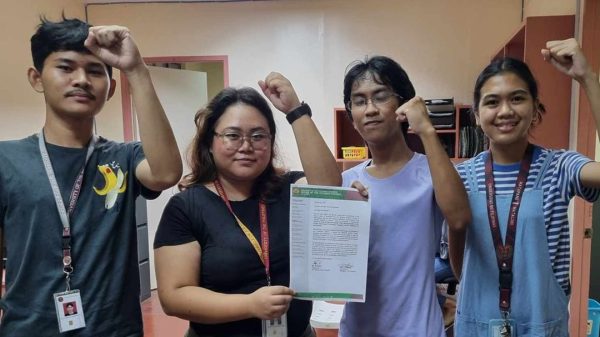
Transgender people are subjected to discrimination in every sphere of life, including education and employment—only 10% work in the formal economy. But community activism has led to long overdue attention to the rights and realities of transgender people.
Some studies have shown that community empowerment activities among sex workers can increase condom use with clients by three times and reduce HIV infection by more than 30%.
The power to demand
The power to demand gives communities and individuals the power to participate in the decisions that affect them. There have been reports of crackdowns, restrictions and even attacks on groups and campaigns supporting key populations. Some governments refuse to recognize, support or engage community organizations in their national responses to HIV and are subsequently missing out on their enormous potential to reach the people most affected by HIV.
People and communities will end AIDS
The work of community-led organizations is unique and powerful and can have a substantial impact on how the world fairs towards ending AIDS. UNAIDS urges all countries to fully support and enable their community-led organizations, ensure they have a seat at all decision-making tables concerning the health and well-being of their community members and remove any barriers to their active engagement in the response to HIV. Only by fully funding and fully supporting the work of community organizations will the end of AIDS become a reality.