High levels of estrogen associated with hormone therapy changes, along with risk factors such as smoking, may lead to porphyria cutanea tarda (PCT) in transgender women.
This is according to a case study, whose findings add to the increasing body of evidence highlighting the higher risk of skin problems in trans women on long-term hormone therapy.
The case study, “Porphyria cutanea tarda unmasked by supratherapeutic estrogen during gender-affirming hormone therapy”, was published in the journal JAAD Case Reports.
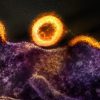
PCT – which is the most common form of porphyria – is caused by a deficiency in the uroporphyrinogen decarboxylase enzyme, which leads to the buildup of porphyrins in the skin, making it extremely sensitive to sunlight.
There are various factors contributing to PCT, including genetic mutations and environmental factors. Some of the factors associated with the disease include: excessive iron levels in the liver, alcohol consumption, smoking, estrogen, hepatitis C, HIV infections, as well as mutations in the HFE gene.
Because of the link of high estrogen levels associated with hormone therapy and PCT, the researchers in the case study suggest for physicians to “recognize the potential risk for PCT in this patient population and consider hormone therapy adjustments, without undermining its importance in affirming gender identity”.
For many members of the trans community, hormone therapy helps affirm their gender identity, potentially easing gender dysphoria (or extreme discomfort caused by a discrepancy between a person’s sex at birth and their gender identity). This, therefore, could help improve quality of life.
But such therapy can also lead to unwanted skin-related side effects, including acne, changes in hair distribution or density, and skin darkening.
In trans women in particular, hormone therapy involves higher estrogen doses than those used for other indications. This is a cause of concern due to risk for conditions associated with estrogen exposure, including PCT.
Physicians should “recognize the potential risk for PCT in this patient population and consider hormone therapy adjustments, without undermining its importance in affirming gender identity”.
The researchers – Stephanie Jackson Collision, Jaroslaw Jedrych and Alaina James – particularly reported on the case of a 55-year-old trans woman who developed PCT following a change in hormone therapy that led to estrogen levels above the therapeutic range (supratherapeutic).
This woman was admitted to the hospital with a three-month history of burning pain, itching, and recurrent blisters on her hands and forearms after exposure to sunlight.
Though she had no personal or family history of liver disease, iron abnormalities, or blistering eruptions, the woman was a smoker and reported drinking two beers a day.
While she had been taking oral estradiol (the most active form of estrogen) daily for the past 23 years, her hormone therapy changed one month before symptom onset. To better control gender dysphoria, she began a trial of oral progesterone (100 mg/day), the other main female hormone, and increased her daily estradiol dose from 2 mg to 4 mg.
Analyses revealed supratherapeutic total estrogen levels (1945 picograms/mL; therapeutic range: 600-1000 picograms/mL), high levels of porphyrins in the blood and urine, and a mutation in the HFE gene.
Overall, the evidence pointed to PCT, likely induced by a combination of supratherapeutic estrogen and other known risk factors, such as tobacco and alcohol use, and HFE mutations.
Attending physicians recommended she stopped taking oral progesterone and temporarily interrupt estrogen therapy, followed by a dose reduction. The woman was also advised to quit smoking, lower her alcohol consumption, and avoid sun exposure.
Clinical remission was achieved within five months without reductions in tobacco or alcohol use. At that time, the woman was reintroduced to hormone therapy with skin patches of 0.025 mg estradiol twice weekly, without PCT recurrence.
For many members of the trans community, hormone therapy helps affirm their gender identity, potentially easing gender dysphoria (or extreme discomfort caused by a discrepancy between a person’s sex at birth and their gender identity).
“The current lack of clear evidence-based hormone therapy (HT) treatment algorithms and barriers to HT access foster therapeutic inconsistency and hormone level fluctuations, which increase the risk of PCT and other cutaneous side effects of HT in transgender females,” the researchers wrote. “It is important to recognize the potential risk for PCT in this growing demographic and consider a multifaceted treatment approach that includes HT adjustment as a therapeutic option, while being mindful of its important role in affirming gender identity.”