October highlighted the continuing disturbing worsening HIV situation in the Philippines, with an estimated 32 new HIV cases now happening in the country every day. For October, there were 1,072 new HIV cases reported to the HIV/AIDS & ART Registry of the Philippines (HARP).
It was in September when this number (i.e. 32 new HIV cases per day) was first reported. Prior to that, the country “only” had 31 new HIV cases reported daily, though even this figure was already considered high compared to figures from past years. In 2009, the country only had two new HIV cases per day. By 2015, the number increased to 22; and in the early part of 2018, the number was 31.
From January 1984 (when the first HIV case was reported in the country) to October 2018 (when the latest figures were belatedly – as usual – released by the HARP), the Philippines already had a total of 60,207 HIV cases. It is worth noting that 9,605 of that figure was reported from January to October 2018 alone.


MALES IN FOCUS
Those newly infected continue to be male – in October, of the 1,072 newly infected, 1,016 (95%) were male. The median age was 28 years old (age range: 2 – 67 years old). Half of the cases (50%, 537) were 25-34 years old and 29% (306) were 15-24 years old at the time of testing.
GEOGRAPHICAL DISTRIBUTION
Based on where those who tested HIV-positive originated, one third (32%, 343) were from the National Capital Region (NCR). Region 4A (17%, 187 cases), Region 3 (11%, 121), Region 7 (8%, 82), and Region 6 (7%, 76), round off the top five regions with the most number of newly diagnosed cases for the month, together accounting for 75% of the total.
Sexual contact remains the main mode of transmission (97%, 1,044). Among this, 86% were males who have sex with males (MSM). Other modes of transmission were needle sharing among injecting drug users (1%, 15) and vertical (formerly, mother-to-child) transmission (<1%, 2). There were 11 cases that had no data on mode of transmission.
Among the newly diagnosed females in October, eight were pregnant at the time of diagnosis. Five cases were from NCR and one case each from Regions 3, 4A and 7.

ACCESSING TREATMENT
In October, there were 831 patients who were initiated on antiretroviral therapy (ART). This is close to the figure registered in September, when 804 patients were initiated on ART. To date, a total of 32,324 people living with HIV (PLHIV) are on ART as of October; and this figure is still only a few thousand over the total number (60,207) of those who reported to have HIV in the country.
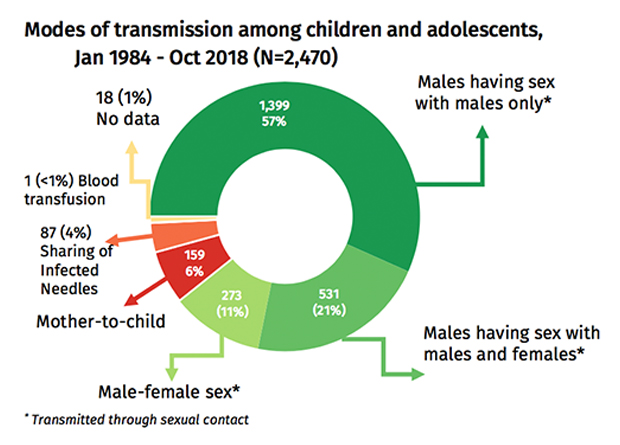
FOCUS ON THE YOUNG
Those getting infected continue to be also younger.
In October, 306 (29%) cases were among youth 15-24 years old; 94% were male. Almost all (98%, 300) were infected through sexual contact (31 male-female sex, 197 male-male sex, 72 sex with both males and females). There were six cases that had no data on mode of transmission.
There were also 41 newly diagnosed adolescents 10-19 years old in October. Almost all (95%) were infected through sexual contact (3 male-female sex, 31 male-male sex, and 5 had sex with both males and females); two had no data on mode of transmission. There were two newly diagnosed child less than 10 years old, and both were infected through mother-to-child transmission.
OFWs IN FOCUS
Even among overseas Filipino workers who tested HIV-positive, more were infected from male-to-male sexual contact.
Eighty-one people who worked overseas within the past five years of diagnosis, whether on land or at sea, were diagnosed HIV-positive in October. They comprise 8% of the total newly diagnosed cases for the month. Among them, 89% (72) were male. Almost all were infected through sexual contact (27 male-female sex, 32 male-male sex, and 21 sex with both males and females). The ages of male OFWs ranged from 23 to 55 years (median: 32 years). More than half (57%) of the cases belonged to the 25-34 year age group. Among the female OFWs diagnosed in October 2018, four cases were from the age groups 25-34 and 35-49; and one case was from 50 years old & older age group. The age range among diagnosed female OFWs were 28 to 61 years (median: 35 years).
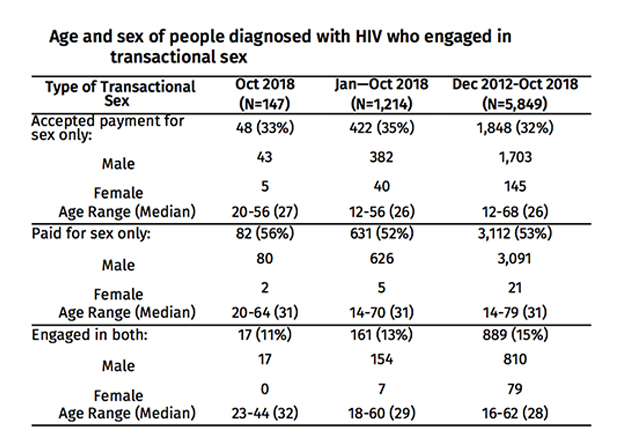
ENGAGEMENT IN TRANSACTIONAL SEX
In October 2018, 14% (147) of the newly diagnosed engaged in transactional sex. Ninety-five percent (140) were male and aged from 20 to 64 years old (median: 30 years). More than half of the males (57%, 80) reported paying for sex only, 31% (43) reported accepting payment for sex only and 12% (17) engaged in both. Among the female cases who engaged in transactional sex, majority (71%, 5) were reported accepting payment in exchange for sex and 29% (2) reported paying for sex only.
Reporting on people who engage in transactional sex – or those who reported that they either pay for sex, regularly accept payment for sex, or do both – was only included in the HARP starting December 2012.
PREGNANT AND HIV-POZ
In October 2018, eight newly diagnosed cases were reported to be pregnant. Five were from NCR and one each from Regions 3, 4A and 7. The age of diagnosis ranged from 19 to 34 (median age: 23).
Reporting of pregnancy status at the time of testing was included in the HARP from the year 2011.
DEATHS AMONG PEOPLE WITH HIV
In October 2018, there were 30 reported deaths due to any cause among people with HIV. Ninety-seven percent (29) were males. One case (4%) was less than 15, four cases (13%) were 15-24, 12 cases (40%) were from 25-34, 10 cases (33%) were from 35-49, and three cases (10%) were 50 years and older age group. Almost all of the cases were reported to have acquired the infection through sexual contact (97%) (3 through male-female sex, 19 through male-male sex, and seven through sex with both males and females); while one case (3%) was infected through vertical transmission.
The 30 deaths are lower than the number reported in August, with reached 159 HIV-related deaths. But the figures are still believed to be be higher because of under- or non-reporting.