He popped a pill. Or probably two. And it wouldn’t have mattered – except that he was in the middle of a dance floor, a weird spot to take medication. He saw me look. He smiled, winked, then turned to make small dance steps. Half an hour later, he was on a ledge, took his shirt off, tucked it in his back pocket, then danced, this time wildly, without a care as he shook, swayed, gyrated, whatever, eyes closed as if in concentration. When somebody banged against him, his eyes opened – and I expected a fight to erupt. But he was smiling. Widely. “Sorry,” the offender said. “It’s okay,” he said. “Everything’s cool!” And then he was back to his dancing. Much, much later, when people were already starting to leave, he was still on the dance floor, extra nice to everyone, incessantly stating “I love you!”. And he looked like he meant it.
He popped a pill. Or probably two. And it wouldn’t have mattered – except that he was in the middle of a dance floor, a weird spot to take medication. He saw me look. He smiled, winked, then turned to make small dance steps. Half an hour later, he was on a ledge, took his shirt off, tucked it in his back pocket, then danced, this time wildly, without a care as he shook, swayed, gyrated, whatever, eyes closed as if in concentration. When somebody banged against him, his eyes opened – and I expected a fight to erupt. But he was smiling. Widely. “Sorry,” the offender said. “It’s okay,” he said. “Everything’s cool!” And then he was back to his dancing. Much, much later, when people were already starting to leave, he was still on the dance floor, extra nice to everyone, incessantly stating “I love you!”. And he looked like he meant it.
“Took E,” somebody said.
And he must have. He looked happy. No, he didn’t just look it, he was happy. And I guess that was all that mattered to him then.
THE PARTY DRUG
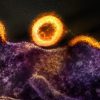
Ecstasy – a.k.a. E, Adam, Bean, M, Roll, X, XTC, Playboy bunnies, Nike swoosh and CK, among others – is one of the most popular drugs among young people today, with an estimated 10 million people – 2.8 million of them teenagers – having tried the drug at least once, and many becoming regular users afterwards (2002 National Survey on Drug Use and Health). This is no wonder because, although even simple possession (much more pushing) of the drug is highly illegal, the designer drug gives temporary justice to its name by giving feelings of emotionally based love and empathy, expansive sense of well-being, ego softening, neurotically based fear dissolution, heightened present moment awareness, and a high that interrupts the feeling of fatigue and tiredness allowing the person to be active all day and into the night – all without visual effects (hallucinations) so lucidity is retained.
Interestingly, even with all the hullabaloo surrounding it, E was an unplanned by-product of the synthesis of Hydrastinin, a vasoconstrictive, and styptic medicine (Methylenedioximetamphetamine or MDMA) by the German Merck Company in 1912. Since then, it has been used as an appetite suppressant, cure to Parkinson’s disease, a possible truth serum, psychedelic therapy drug, and a reducee of hostility in marriage counseling sessions. Sometime in those years, E started to be used for “recreation.”
From that time on, E was on its way to infamy.
While it has become a controlled substance (only licensed physicians may prescribe it), illegal possession of which carries the stiffest penalties (even death), the number of users continue to grow every year, as if proving the local saying Masarap ang bawal. Thus, it is always worth giving attention to – not to promote it, but because even with the accompanying risks, there are those who’d still use it, and knowledge (not just prohibition) alone may save them.
THE GOOD AND THE BAD
There are numerous misinformation about E, e.g. that it causes Parkinson’s disease (a confusion between MDMA and MPTP); or that users simply fall while dancing (people have actually died from heatstroke while at raves on E, but caution and use of common sense could prevent this).
Taking effect in as less as 30 minutes, with two to three hour plateau, and then six hours to baseline, E is popular because of its effects. There’s entactogenesis (touching within), a generalized feeling that all is right and good with the world. Empathogenesis, a feeling of emotional closeness to others (and to one’s self), coupled with a breakdown of personal communication barriers. An enhancement of the senses, since E can significantly enhance (sometimes distort) the senses – touch, perception, vision, taste, smell. Prolonged stamina, with users dancing ‘til the wee hours of the morning. And, since E can catalyze a broad range of psychotherapeutic effects (surfacing of repressed memories, dealing with emotional issues, et cetera), alternative psychotherapy.
With a detection period of one to two days (though generally depending on the amount and frequency of usage), E, nonetheless, has been known to have numerous ill effects.
While the physical effects of usual doses of E are subtle and variable (including dryness of mouth, jaw clenching, teeth grinding, nystagmus (eye wiggles), sweating, shivering, tremor or nausea), E causes an increase in blood pressure and pulse rate, modest in most people, similar to moderate exercise, so that people with a history of high blood pressure, heart trouble, or stroke are advised not to use E, or at the very least are advised to start with a much lower than average dose. Liver or kidney problems. Loss of appetite. Mild to moderate post-session fatigue. Lessening of the awareness of pain (whether through chemical analgesia, or through psychological analgesia), so bodily damage from extensive dancing, hiking, climbing, et cetera, without noticing it until after the damage is done. Inhibition of serotonin reuptake (though this could be prevented by taking anti-oxidants). Possible internal hemorrhage (E has anticoagulant properties that can cause this). And Psychoses.
Taking the drug is, then, at your own risk.
KNOWLEDGE IS POWER
This is not an encouragement to take E, but at least if/when you do, be safe doing so.
- Avoidance is the first advice. But since many avoid the avoidance recommendation, check physical condition before using, since E puts serious strain on the body.
- If you feel that you are uneasy about taking it, and not comfortable with being that open with yourself and having your image stripped from you, then don’t do it.
- Find a situation you feel comfortable and safe in – and find someone you can trust.
- Drink as much water as you like, but avoid alcohol (while it’s not going to kill you or make you sick, alcohol will deaden the effect of the drug) and other drugs (combining with any kind of speedy drugs like cocaine, shabu, et cetera can kill you).
- If you are dancing, realize that you may be dangerously overheated even without feeling uncomfortable. Look after friends and get them to look after you. Taking vitamin C and E may help reduce exhaustion. Get good sleep afterwards.
- Don’t take more than one pill or take it more than once a week. Your body builds a tolerance to X very quickly.
The drug is HIGLY ILLEGAL, and, if caught, you will be jailed and be even sent to die by lethal injection just for a brief moment of ecstasy.
You have been warned. Now learn the truth for yourself and make up your own mind about E before taking it.
REFERENCES:
Toxicology Associates, Inc.
National Institute on Drug Abuse
www.a1b2c3.com/drugs/#ecstasy
American Journal of Forensic Medical Pathology
Neurology Journal
csdp.org
DanceSafe.org
maps.org