The Philippines now has a new law eyeing to strengthen the country’s comprehensive response against HIV and AIDS
People may already be familiar with RA 8504, or the Philippine AIDS Prevention and Control Act of 1998. When it was introduced, RA 11166 or the Philippine HIV and AIDS Policy Act intended to update Republic Act 8504 to incorporate lessons from the current HIV response by introducing “newer evidence-based, human rights-informed, and gender transformative strategies to prevent and treat the epidemic.”
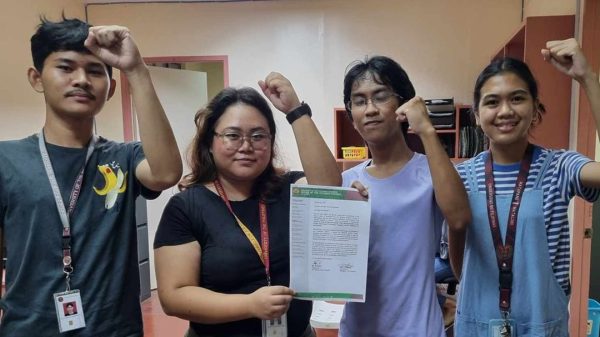
The Philippine HIV and AIDS Policy Act was ratified by both the Senate and the House before Congress went on recess on October 10, 2018. It was then transmitted to Pres. Rodrigo Duterte on November 26, 2018
Some of the new law’s eminent features include:
- Minors aged 15 to under 18 may now voluntarily get tested for HIV, as stated in Article IV, Section 29 (versus the need for approval of their parents or guardians, as previously required under Republic Act 8504).
- Mandate for the Department of Health (DOH) to establish a program that would provide free and accessible anti-retroviral treatment and medication for opportunistic infections to people living with HIV who would enroll in the program.
- Mandate for the Philippine Health Insurance Corporation to develop a benefit package for PLHIVs to include coverage for inpatient and outpatient medical and diagnostic services, including medication and treatment. It is now prohibited by law to deny PLHIVs private health and life insurance coverage and claims.
- Development of basic and age-appropriate instruction on the causes, modes of transmission and prevention of HIV, AIDS and other sexually-transmitted infections in public and private schools, including alternative and indigenous learning systems.
- Mandate for the Department of Education to conduct awareness-building seminars in coordination with parent-teacher organizations to provide parents and guardians with a “gender-responsive and age-sensitive HIV and AIDS education.”
- Provision of education on HIV and AIDS shall to all public and private employers and employees, members of the military and police, overseas Filipino workers, communities and key populations at higher risk for infection.
- Jail term of six months to two years and/or a fine of not less than ₱50,000 on anyone who discloses the information that a person has AIDS, undergone an HIV-related test, has HIV or HIV-related illnesses or has been exposed to HIV, without their written consent.
- Prohibition of disclosure of the name, picture or any information that would identify people living with HIV and AIDS or any confidential HIV and AIDS information on media without their written consent. The mass dissemination of these confidential information would be punished with imprisonment for two years and one day to five years, and/or a fine of ₱150,000 to ₱350,000.
- Jail term of six months to five years and/or a fine of ₱50,000 to ₱500,000 for those discriminating against PLHIVs; and may have their business permit, business license or accreditation or professional license suspended or revoked.
Incidentally, the Philippines has the fastest growing HIV epidemic in the Asia-Pacific, with infections jumping by 140% from 2010 to 2016. The country currently records 32 new HIV cases every day, though responses to this have varied – e.g. the DOH has been criticized for complaining about budget cuts, and yet spending money on a beauty pageant; while there are NGOs criticized for putting profit before service in HIV-related efforts.
Following the signing of the Philippine HIV and AIDS Act by Duterte, Secretary of Health Francisco T. Duque III released a statement via the media relations unit of the DOH stating that “the signing of the Philippine HIV and AIDS Act is a huge step forward in responding to the growing HIV epidemic in the Philippines” because now, “mabibigyan na natin ng tamang suporta ang mga Pilipinong may HIV-AIDS (we can give proper support to PLHIVs).”
But the sentiment may be put in bad light because of the ongoing ARV shortage affecting the HIV community, wth a growing number of Filipino PLHIVs now lamenting: 1. not receiving regular supplies of ARVs (some allegedly getting meds only for a week or even three days, instead of the usual three months’ supply); 2. being shifted to another ARV because their usual/regular medicines are not available due to procurement issues by the DOH; or 3. being made to use expired medicines because there are no other available medicines for them.
With the new law, the next step is now to develop and then properly execute an Implementing Rules and Regulations to guide executive officials in implementing the law, as well as the public in how to comply with the law.
UPDATED ON JANUARY 9: An earlier version of this article stated that the the HIV and AIDS Policy Act lapsed into law, 30 days since it was transmitted by Congress to Malacañang, where Pres. Rodrigo Duterte failed to sign it. Laws transmitted to Malacañang which are not acted on for 30 days lapse into law; and initially, it was thought that Duterte neither signed nor vetoed the HIV and AIDS Policy Act, therefore it lapsed to becomes the country’s new HIV-related law. However, the copy of the RA 11166 released by Malacañan Palace shows that the law was actually signed by the President on December 20, 2018.