This is part of “More than a Number”, which Outrage Magazine launched on March 1, 2013 to give a human face to those infected and affected by the Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDS) in the Philippines, what it considers as “an attempt to tell the stories of those whose lives have been touched by HIV and AIDS”.
More information about (or – for that matter – to be included in) “More than a Number”, email editor@outragemag.com, or call (+63) 9287854244 and (+63) 9157972229.
BACKGROUND: While working as a nurse in Abu Dhabi, United Arab Emirates, @pozzieblue tested HIV-positive in July 2013. He was placed in an isolated facility in the middle of a desert, and then deported to the Philippines. Months after trying to get his life back together, he shared his story to Outrage Magazine in November 2013. This is a new contributed article from him, sharing how life has changed for him after he tested HIV-positive; and the lessons he hopes others like him learns from life.
After being detained and deported, life was not easy. I felt I’ve went back to zero. I grieved a lot, and sometimes I thought I’ve reached the acceptance phase but the anger and sadness fluctuates every now and then. There was even a time that I went to RITM from my hometown by myself, and I was still struggling from my pneumonia and ARV allergic reaction. I needed to go back to my hub so I could refill my new ARV. I was on MRT train when I felt I was fainting so I’ve decided to sat on the floor to gain my strength and to avoid falling. It felt so terrible and lonely because as a nurse who used to take care different people, nobody cared to approach and ask me if I’m okay.
This is the reason why I realized that I need to focus on one of the most important aspect of my life, my health. Later on, I discovered twitter. I am grateful because this social media became a great support system to me because the of the fellow poz who have their account there. They have been very encouraging to my PLHIV journey, so I’m truly thankful to them. In fact, I have found some of my true best friends.They were there in supporting me in different ways, specially to my mental health.
When my health became stable, I started working from different fields. I hopped from the BPO industry, teaching International students and doing online jobs. I was upset because it was hard to start a clean slate. Maybe because deep in my heart, I hold this faith that there is still another world waiting for me, but this virus in my blood inhibits me, as well as the trauma I’ve had. Then I promised myself that my life will not end this way and just like the long-time drama anthology says “Ikaw ang bida ng buhay mo.”
I tried enriching my neurons by finishing my Master’s Degree and improving my English skill. I was spending my earnings in different classes and dealing my thesis. During that time, I was also rekindling my relationship to God. There was a time that I felt He left me, but I realized that during those lowest lows of my life, he was there all through out, but I couldn’t see him because I was blinded with frustration, anger and regrets.
After going through with my Master and passing my English test. I’ve received an information from another PLHIV that he knows a nurse who was accepted to work in UK to practice his profession, despite being a poz. That simple online conversation ignited a hope in my heart. Hence, I started applying for an overseas job again. I can still remember how much worry it caused me whenever I needed to disclose my HIV status to my prospective employers but I’m grateful that they don’t mind it.
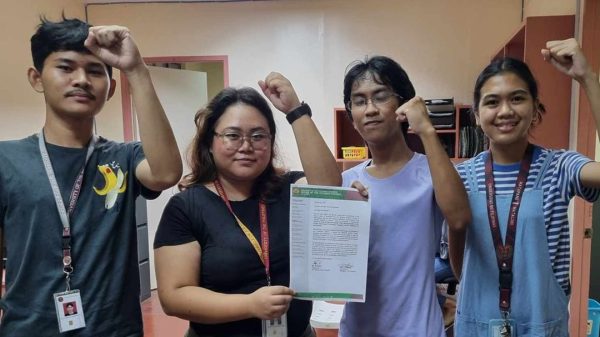
To make the story short, I’m now in UK and I just passed my final exam to become a Registered Nurse here few weeks ago. It wasn’t an easy journey, but with perseverance, good health and divine intervention; I was able to fulfill this dream. I remember what Pope Francis said, “When you lose the capacity to dream, you lose the capacity to love, and the energy to love is lost.” This is my new mantra now.
To all my fellow PLHIV out there: life may seem to be a continuous struggle but continue learning and enriching yourself. Ask for help if you think you need one. Pain and sorrow is subjective. I may not know what you are going through but I sincerely wish everyone well.