“Three of my closest friends committed suicide last week,” John Albert shared in a post. “I could not believe the news when I heard it. I saw them before the lockdown; everything seemed fine.”
I chatted with John Albert, and in a short online conversation, he said that one of these friends was a lesbian. Her body was reportedly found by a barangay tanod who was patrolling their area. When they checked the phone beside her, there were 30 missed calls and 57 unread notifications. According to John Albert, the last message his friend sent was to her brother: “Ang hirap pala ng ganito, nag-iisa ka lang at wala kang makausap. Nalulungkot ako pero wala akong choice. Sana matapos na itong lockdown.”
But John Albert’s lesbian friend isn’t the only such case – at least it seems – of members of the LGBTQIA community dealing with the mental strife brought about by the Covid-19 pandemic.
Tere, a transgender woman who started her transition this January, lives in a small apartment and is used to doing things on her own, in her own way. But it changed on March 17, when Pres. Rodrigo Roa Duterte enforced the Enhanced Community Quarantine (ECQ) in Luzon, which halted just about everything.
Most people were forced to adjust to what is only available. And in Tere’s case, this meant “temporarily” moving back to her parents’ house. And there, she does not exactly feel fully welcomed.
“For some reason, my father always scolds me. He wants me to do this and that, always asking me questions about my decision to transition and what will happen to my future,” shared Tere, who lamented that all her movements are being monitored so she cannot do her usually routine. “It had already come to a point that I just stay in my room the whole day and cry. I started questioning myself, too.”

Photo by Alan Cabello from Pexels.com
FOCUS ON MENTAL STATE
“The new normal” – as people are now referring to the time of Covid-19 – is also testing how strong one’s coping mechanism is, particularly with the need to socially isolate that could trigger loneliness, which the American Psychological Association says increases the risk of premature mortality.
After all, two of the major factors that may contribute to a person’s mental health is the sudden change in physical and social environments. And so: What if you are someone who is struggling to manage how you think, feel and behave given the current controlled environment?
At this point, there’s the acknowledgement that the Covid-19 pandemic not only attacks the body’s immune system, but also wreaks havoc on the mental state of people.
A recent chat with Filipino persons living with HIV (PLHIV), for instance, showed that aside from the paranoia about the disease (e.g. how it spreads, the constant danger of being in close contact with someone who has it), the battle with one’s self can just be as difficult.
Sadly, there are no available outlets to release these anxieties, just the confines of your home/room/house. And for many, this is proving to be very difficult.
Perhaps even more so for LGBTQIA people going through additional difficulties because of their sexual orientation, gender identity and/or gender expression.
LOOKING FOR A WAY OUT
John Albert’s lesbian friend’s demise highlights how bad things can turn out.
And suicide isn’t “rare” in the Philippines – even if still not as widely discussed. In 2016, the World Bank reported that the Philippines’ suicide rate was 3.20 per 100,000 inhabitants. The rate has actually been growing since 2000.
And as the country slowly copes with the “new normal”, the issue of mental health continues to be in the back burner. “Priorities” now continue to focus on: controlling the spread of Covid-19, and mitigating its impact on the economy.
In a paper published in Lancet Psychiatry, scientists already stressed the need to also prioritize mental health, since a crisis could have “profound” and “pervasive impact” on global mental health now and in the future.
The World Health Organization (WHO), itself, acknowledged that “as the coronavirus pandemic rapidly sweeps across the world, it is inducing a considerable degree of fear, worry and concern in the population at large and among certain groups in particular…”
WHO stressed that: “In public mental health terms, the main psychological impact to date is elevated rates of stress or anxiety. But as new measures and impacts are introduced – especially quarantine and its effects on many people’s usual activities, routines or livelihoods – levels of loneliness, depression, harmful alcohol and drug use, and self-harm or suicidal behavior are also expected to rise.”
But there are steps that can be taken.
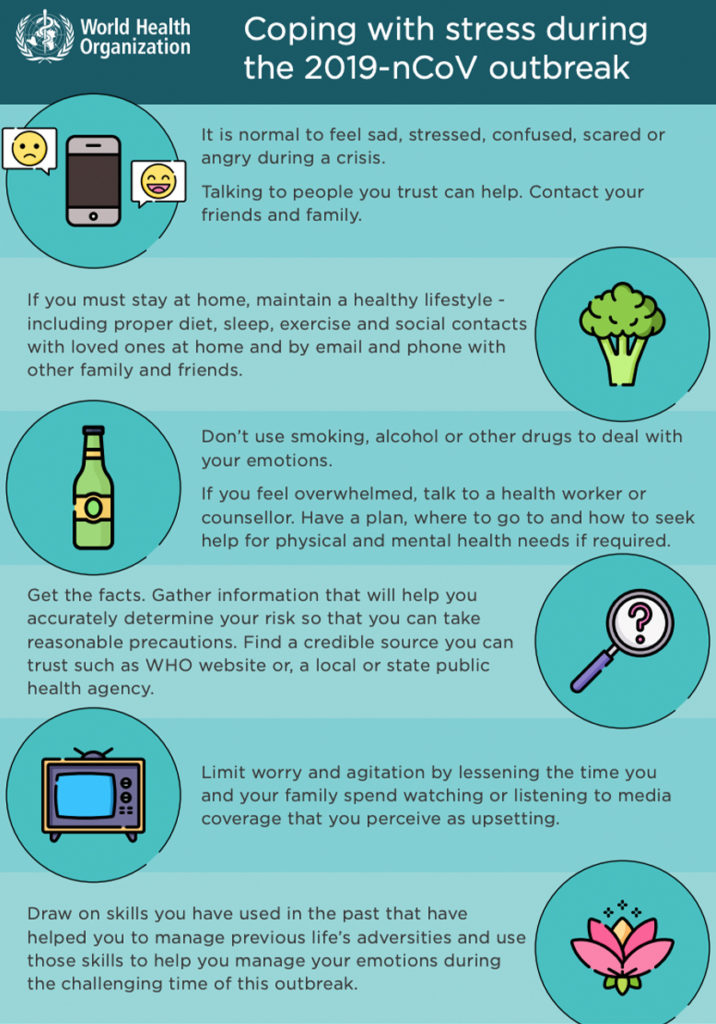
US-based Centers for Disease Control and Prevention (CDC) added practical ways to cope with stress:
- Take breaks from watching, reading, or listening to news stories, including social media. Hearing about the pandemic repeatedly can be upsetting.
- Take care of your body.
-
- Take deep breaths, stretch, or meditate.
- Try to eat healthy, well-balanced meals.
- Exercise regularly, get plenty of sleep.
- Avoid alcohol and drugs.
- Make time to unwind. Try to do some other activities you enjoy.
- Connect with others. Talk with people you trust about your concerns and how you are feeling.
It is worth stressing that for those dealing with mental health issues, know that there are ways to lessen the stress and burden on the mind. And perhaps apt to stress is the need to help each other. Just as Cebu City-based transgender woman Magdalena Robinson, CEO of the Cebu United Rainbow LGBTIQ+ Sector Inc., said, this is the right time to “fix each other’s crown.”